My Village of Breastfeeding Support
Over the next few weeks we will be sharing stories of triumphant breastfeeding mamas and their biggest supporters who helped them reach their personal breastfeeding goals. If you would like to share your breastfeeding story and thank your biggest breastfeeding cheerleaders, check out the details in our recent blog article.
_____
Here is Stephanie's story.
It has truly taken a village to help me be successful in nursing both of my babies! I knew I wanted to breastfeed, but, after the birth of my first son, my passion and commitment to it were a surprise to even me. I was also caught extremely off-guard by the difficulties both of my boys encountered as we began our breastfeeding journeys together. Tongue ties, lip ties, low weight gain, low supply, poor latch, pain/cracking/bleeding, overactive letdown, and more were all hurdles we had to cross. There is absolutely NO way I could have made it to 13 months formula-free with my first son and still going strong and formula-free at 6 months with my second without these amazing people.
Over the next few weeks we will be sharing stories of triumphant breastfeeding mamas and their biggest supporters who helped them reach their personal breastfeeding goals. If you would like to share your breastfeeding story and thank your biggest breastfeeding cheerleaders, check out the details in our recent blog article.
_____
Here is Stephanie's story.
It has truly taken a village to help me be successful in nursing both of my babies! I knew I wanted to breastfeed, but, after the birth of my first son, my passion and commitment to it were a surprise to even me. I was also caught extremely off-guard by the difficulties both of my boys encountered as we began our breastfeeding journeys together. Tongue ties, lip ties, low weight gain, low supply, poor latch, pain/cracking/bleeding, overactive letdown, and more were all hurdles we had to cross. There is absolutely NO way I could have made it to 13 months formula-free with my first son and still going strong and formula-free at 6 months with my second without these amazing people.
My husband! My passion and commitment to breastfeed my babies surprised him also, but he never questioned it and stood by me no matter what decisions I made! He became just as committed and passionate about it, knowing it was the best thing we could do for our boys. He came to appointments, helped get the baby latched on time after time, stood up for me when others questioned why I didn’t just quit, and let me cry when it all just became too much! He has truly been my rock through all of this, and I can sense his gratitude for the sacrifices I have made to give our boys this amazing gift!
My Lactation Consultants! Four different lactation consultants have come alongside my babies and me in our journey together. Every single one of them encouraged me that I could do it when the hurdles seemed insurmountable. They provided a listening, sympathetic ear when I just needed to vent or cry or talk it out. They provided help, advice, referrals, and life-changing solutions that kept us going!
My tribe of other breastfeeding Mamas! Friends I have known since childhood, friends I’ve made in recent years, and people I met through the breastfeeding process made it all possible - others who had or were experiencing some of the same challenges, some who didn’t have trouble but believed just as passionately in the benefits of breastfeeding, some who visited, some who called, and one who even created an on-line community to connect us all! There were many people in my life who didn’t understand why I didn’t give up when they saw the emotional and physical toll it was taking on me, but these other Mamas got it! They knew why I couldn’t quit, why no challenge was too big!
My virtual breastfeeding community! Although I will never meet most of these women in person, the support, advice, commiseration, and encouragement they have provided have truly been critical! To be able to jump online in the middle of the night when it just seemed like I couldn’t do it and have others on there to tell me that, yes, I could do it got me through many rough moments! They have calmed nerves, answered questions, given virtual hugs, and just been an amazing support system!
My babies! Even from the very start and even in the face of all of our challenges, my babies have always loved nursing! They didn’t quit so there was no way I could!
Breastfeeding in the Operating Room
Over the next few weeks we will be sharing stories of triumphant breastfeeding mamas and their biggest supporters who helped them reach their personal breastfeeding goals.
_____
This story is from Dawn.
I have to thank my hospital TEAM for my breastfeeding success!
When I gave birth to my son 5+ years ago, it wasn’t what any first time mom would like to experience. I was having problems with maintaining my blood pressure and when my little boys’ heart rate dropped too low, I was rushed into an emergency c-section. It was an extremely frightening process that didn’t even enter my mind as a possibility. The months that followed were hard. We struggled at finding a proper latch and feeding became such a difficult task, I dreaded it.
It never occurred to me that our difficulties at latching could have been because of the birth experience .
Over the next few weeks we will be sharing stories of triumphant breastfeeding mamas and their biggest supporters who helped them reach their personal breastfeeding goals.
_____
This story is from Dawn.
I have to thank my hospital TEAM for my breastfeeding success!
When I gave birth to my son 5+ years ago, it wasn’t what any first time mom would like to experience. I was having problems with maintaining my blood pressure and when my little boys’ heart rate dropped too low, I was rushed into an emergency c-section. It was an extremely frightening process that didn’t even enter my mind as a possibility. The months that followed were hard. We struggled at finding a proper latch and feeding became such a difficult task, I dreaded it.
It never occurred to me that our difficulties at latching could have been because of the birth experience.
In early 2012 we received good news, we were expecting! I did my best to set everything up for a different birthing experience. I searched out a CDC accredited Baby Friendly Hospital in my area, researched VBAC’s and educated myself on the benefits of skin-to-skin. It wasn’t until closer to my due date that I was informed I couldn’t have a VBAC. No hospital would even consider me as a potential VBAC candidate because of my small heart issue as well as my age. After fighting and pleading, I had to acknowledge that I had no other option, but another C-section.
I may have lost that battle, but I was going to do everything in my power to have skin-to-skin with my little girl. I was aware of the evidence-based research on the benefits of skin-to-skin and its success rate with c-section births. I talked to my pediatrician about this and he agreed. (I since found out that it is the pediatrician who is in charge in the OR!) I wrote my birth plan with the intentions of doing skin-to-skin immediately after the c-section unless there was a medical reason not to.
Alas, I wasn’t able to make it all the way to my scheduled c-section date. This time I was low on amino fluids and baby’s lack of movement put me into the hospital at 36 weeks. With concern, my OB and the pediatrician, agreed, that under supervision, they would monitor me and try to get us to the 37th week and do the c-section.
Now, prior to this, we made sure to talk with all the right people about our wishes for skin-to-skin. Everyone was on board: our OB, the hospital’s labor and delivery nurses, and staff. In fact, the hospital staff has been championing the change in procedures to allow skin-to-skin in the OR without success.
The day of my C-section, my regular pediatrician was out of town and his standing replacement wasn’t comfortable at all. I had to conveince the standing pediatrician that this was in my and my baby's best interest. The hospital's Head Labor & Delivery nurse helped us get to a compromise! She is my angel! She proposed that if everything looked good my little girl would be immediately placed on my chest, without ANY other intrusion.... meaning the vernix would be wiped off her while she was on my chest and she would be weighted and measured later.
When the hour came for us to have the c-section more drama around skin-to-skin unfolded, this time all the way up to the director of the Family Birth Center. The director of the Family Birth Center was completely opposed to it and tried talking my OB out of it. We were lucky we had enough support and commitment from the labor and delivery nurses and my OB to move forward. We finally got our wish!
I have to admit, because she was coming 3 weeks early, I wasn’t sure we would even get the option of skin-to-skin, but our little girl emerged perfectly! She was screaming and quickly confirmed in perfect health!
When she was placed on my chest and covered with a warming blanket, I was in awe. This little 6 pound bundle was just perfect. After a little while, she actually scooted and rooted for my breasts and eventually latched and nursed! I just didn’t think I would get that experience since she was early. The remembrance still makes me cry. It was such an amazing experience. I was so happy I had the team in my corner and the hospital went forward with my wishes.
When I was first told I would have to have another cesarean, I felt completely out of control and very disappointed. Creating a birth plan around my c-section allowed me to take a bit of control back and talking with all parties that come with a c-section allowed me the skin-to-skin connection that was deeply important to me.
It has been over a year since Beth was born. We are still nursing strong and have a connection that I attribute to the wonderful team that helped me get skin-to-skin in the OR!
Side note: I have since heard that they have allowed other moms the same experience! The hospital team not only helped me, but also have persevered in getting policy “changed” at the hospital!
Dawn Alva
Comebacks for ‘Why Are You Still Breastfeeding?’
Any woman who has ever had a breastfeeding challenge or has breastfed longer than than someone else deems ‘normal’ has been asked this question at one time or another.
“Why are you still breastfeeding?”
Sometimes this question is passive aggressive with undertones of “I can’t believe you have breastfed your baby for THIS long.” Other times it comes from a place of love meaning “You seem like you are in pain... are you sure you still want to try this?”
Regardless, if you are anything like me, the snappy comeback or educated response that I SO desired to say only comes after the situation is long gone and I am kicking myself for not defending myself and my choice to breastfeed the way I wanted to.
Any woman who has ever had a breastfeeding challenge or has breastfed longer than than someone else deems ‘normal’ has been asked this question at one time or another.
“Why are you still breastfeeding?”
Sometimes this question is passive aggressive with undertones of “I can’t believe you have breastfed your baby for THIS long.” Other times it comes from a place of love meaning “You seem like you are in pain... are you sure you still want to try this?”
Regardless, if you are anything like me, the snappy comeback or educated response that I SO desired to say only comes after the situation is long gone and I am kicking myself for not defending myself and my choice to breastfeed the way I wanted to.
Well, ladies... look no further!
Here are some handy, snappy (evidence-based) comebacks that you can tuck away in your back pocket, only to whip out at the most appropriate times, pun intended! (P.S. These comebacks also work if someone asks why you are STILL exclusively pumping!)
Top 10 Comebacks to Answer the Question: Why Are You Still Breastfeeding?
1. “It’s the perfect food for my child. 24 hours a day, 7 days a week!”
- Babies can digest human milk more easily than the milk of other animals, probably because human milk contains an enzyme that aids in this process.
- Breast milk forms softer curds in the infant's stomach than cow's milk (the basis for most formulas) and is more quickly assimilated into the body system.
- While it contains less protein than does cow's milk, virtually all the protein in breast milk is available to the baby. By contrast, about half the protein in cow's milk passes through the baby's body as a waste product.
- Similarly, iron and zinc are absorbed better by breastfed babies.
2. “Breastmilk doesn’t lose it’s nutritional value. Can you say that about the food YOU eat?”
- Even at a year, breastmilk continues to pack a powerful punch for nutritional value.
- In the second year (12-23 months), 448 mL of breastmilk provides:29% of energy requirements
- 43% of protein requirements
- 36% of calcium requirements
- 75% of vitamin A requirements
- 76% of folate requirements
- 94% of vitamin B12 requirements
- 60% of vitamin C requirements
Dewey KG. Nutrition, Growth, and Complementary Feeding of the Breastfed Infant. Pediatric Clinics of North American. February 2001;48(1), from Kellymom.com Breastfeeding Past Infancy Fact Sheet
3. “Breastmilk protects against disease for my baby. Don’t you want my (our) baby to be healthy?”
- Because the mother makes antibodies only to pathogens in her environment, the baby receives the protection it most needs-against the infectious agents it is most likely to encounter in the first weeks of life.
- Here are a few ways that breastmilk helps make a healthy baby:
- Breastfed babies also have less diarrhea and fewer gastrointestinal infections than babies who are artificially fed.
- Six months or more of exclusive breastfeeding reduces risk of food allergies.
- Breastmilk decreases a child’s risk of Crohn's disease and ulcerative colitis in adulthood.
- Breastfed babies have lower risk for developing recurrent wheezing when they are older (age 6 or more) – asthma
- They have less reflux
- They have less eczema
- Breastfeeding protects baby against respiratory infections
- Women who were formula-fed as infants have higher rates of breast cancer as adults. For both premenopausal and postmenopausal breast cancer, women who were breastfed as children, even if only for a short time, had a 25% lower risk of developing breast cancer than women who were exclusively formula-fed as infants.
4. “There are incredible health benefits for my breastfed baby. Do you really think it’s wise to limit my baby’s intellectual and physical potential?”
- Breastfed children have higher IQ
- Breastfeeding reduces a baby’s risk of SIDS by 50%
- Breastfeeding protects baby against vision defects. Breast milk is generally the main, if not the only source, of vitamin A during a child's first 24 months of life (or for the duration of breastfeeding).
- Suckling at the breast is good for a baby's tooth and jaw development, as the constant pulling at the jaw muscles promotes a well-formed jaw and healthy teeth.
5. “Breastfeeding improves my overall health. Who’s going to cook all of the meals and take care of the home if I’m not healthy? (I know...super snarky!)”
- Breastfeeding decreases mom’s risk of postpartum hemorrhaging as it stimulates contractions to shrink he uterus back to pre-pregnancy size.
- Breastfeeding reduces mom’s risk of osteoporosis
- Breastfeeding reduces mom’s risk of anemia, as breastfeeding postpones the return of menstruation for many women.
- Breastfeeding reduces mom’s risk of breast cancer. Women who breastfeed reduce their risk of developing breast cancer by as much as 25 percent. The reduction in cancer risk comes in proportion to the cumulative lifetime duration of breastfeeding. That is, the more months or years a mother breastfeeds, the lower her risk of breast cancer.
- Breastfeeding reduces the risk of uterine and ovarian cancer.
6. “Breastfeeding promotes mother/infant bonding and emotional well-being.”
- Babies feed for about 45 minutes per time in the first few months. This is nature’s way of making moms sit down and relax and promote her postpartum healing.
- Breast milk actually contains chemicals that suppress pain (endorphins). This is the perfect remedy for a child who accidentally hurts himself and is in need of some pain relief and comfort. It's like having a boo-boo-healing superpower!
- Babies can also feel the warmth of mom's skin, take in her scent and hear her heart beating. This helps to neurologically center thebaby after birth and help him/her adjust to the outside world.
- Breastfeeding also decreases a mother’s risk for postpartum depression.
7. “Breastfeeding can promote a positive relationship between mom and a supportive partner.”
- Partner support is crucial during breastfeeding, especially when there are challenges along the way.
- In the beginning, when baby is pretty much just eating and sleeping, mom and her partner can spend this time together, hanging out while the baby is feeding, getting to know one another as parents, not just partners.
- This is a great time to reconnect with your partner as the both of you get to know your baby, as this is a new time for your family.
- You are also a team during this time. Partners can make sure that all visitors offer positive breastfeeding comments, especially when breastfeeding is a challenge. No sabotaging comments allowed!
8. “Breastfeeding is definitely more convenient and less expensive than formula. I thought we were on a tight budget!”
- Breast milk, in any supply, is free. Ready-made formulas can cost families $800 to $1800 per child, annually.
- Nipples, bottles, bottle brushes and bottle bag inserts are additional costs, as well.
- Breastfed babies are ill less often, meaning that their parents miss fewer days at work and spend less on prescriptions, doctor's visits, and hospital stays.
9. “Breastfeeding, just like parenting, has bumps along the road and I won’t quit on my worst day.”
- As all thing that have to do with parenting, what works some days, doesn’t work on others and most things don’t go smoothly as planned.
- Your baby is born with a personality and a style that requires becoming familiar with and understanding.
- What works for some babies and children may not work for yours, so seek support anywhere you can find it: friends, family, lactation consultants, websites, Facebook groups, physicians, etc.
- Don’t quit on your worst day. Let 24 hours pass to gain some perspective and reach out for help during that time.
- Have an IBCLC evaluate your situation and provide a plan for overcoming your challenge.
10. “I promise you that my child won’t breastfeed until his high school graduation, but if he did, he’d probably be the smartest, healthiest graduate there!”
- Ok, maybe that’s a little too sassy, but you get the point. It is your choice to breastfeed for as long as mutually beneficial for you and your child. Every drop of breastmilk your child gets is liquid gold and you are a superstar for producing that for him/her! So stay strong, mama, and know that your ‘breast friends’ have your back! Happy nursing!
Help a Mama Out: Nurturing Your Breastfeeding Relationship when Back at Work
Help a Mama Out Topic of the Week: What are your favorite ways to nurture your breastfeeding relationship when you work outside the home?
Sarah – When I was working out of the home, I pumped at the times my daughter would take a bottle. Then, when I came home I would exclusively nurse her. She was fine with 2 or 3 small breastmilk bottles a day, then nursed the rest of the time. She always preferred the breast and when it came time to wean, I was nervous….but at 13 months she just did and that was that!
Alicia – Comfort nursing on the weekends and morning nursing cuddle time. I always nurse as soon as we get home from work/daycare.
Alyssa – My favorite part of my working day (as a teacher) was when I sat down in the glider at daycare and nursed my son before taking him home for the night. We were always so happy to see each other and it helped wipe away any headaches from the day. Plus, I developed a friendship with his teacher and got to hear all about what he did that day, which was way better than just reading a quick note on a daily info sheet!
Jeanne – Co-sleeping helped us and a feed before I leave and ASAP when I get home. I also pump 3-4 times at work and always demand feed when I’m home.
Katie – We nurse in the evenings, when she wakes up in the middle of the night, and at least once more before I leave for work. It’s funny, as soon as I pick her up after work, I think her mind lights up with ‘milk!’ because she immediately wants to nurse regardless of when her last feeding was. I can tell that she misses that when we’re a part, as do I.
Janell – As soon as I get home, he’s on the boob. The rest of the night, he is on the boob. We spend all weekend with him on and off the boob. Time consuming, but I love the connection time and it forces me to sit down and breathe with my son.
Rachel – I sit with my daughter every evening after work. Even if she goes to sleep, we spend the entire evening and night together because we co-sleep. I make a point to forget about all of the housework I have to do and just relax with her because I know that she won’t be little forever!
Rachelle – One of my favorite things is when I get home from work, I shower (I’m a paramedic). After I shower, I fill the bath and my husband brings me the baby and we usually relax and nurse for 20-30 minutes. It is my wind-down time and it is quiet with few distractions. I love it!
Sarah – If possible, try to arrange a mid-day nursing session. I used a local daycare that I was able to visit at lunch and nurse, rather than pump. It greatly helped my supply and we were able to EBF for 13 months without any supplementation.
Amanda – I asked out childcare provider not to feed our little one within 90 minutes of when I planned to pick up. That way I could nurse as soon as I got there.
Breastfeeding Misconceptions: Does Baby Weight Loss Mean Mom Doesn’t Have Enough Milk?
How many times have you heard a so-called ‘fact’ from a family member, friend, healthcare professional, or online resource that has your ‘mama-radar’ going off at warp speed? Maybe something just doesn’t sound right. Maybe it goes against all of your mama-bear instincts. Maybe it is completely contradictory to what you heard the previous day. Well, it’s time to start busting those myths and misconceptions!
Today, we start our new series called Breastfeeding Misconceptions.
Every month we will be BUSTING common breastfeeding myths and misconceptions, hopefully making your breastfeeding experience that much easier!
How many times have you heard a so-called ‘fact’ from a family member, friend, healthcare professional, or online resource that has your ‘mama-radar’ going off at warp speed? Maybe something just doesn’t sound right. Maybe it goes against all of your mama-bear instincts. Maybe it is completely contradictory to what you heard the previous day. Well, it’s time to start busting those myths and misconceptions!
Today, we start our new series called Breastfeeding Misconceptions.
Every month we will be BUSTING common breastfeeding myths and misconceptions, hopefully making your breastfeeding experience that much easier!
Myth #1: If your baby loses weight in the first week, it means your milk supply is low.
Not true!
All babies lose weight after birth:
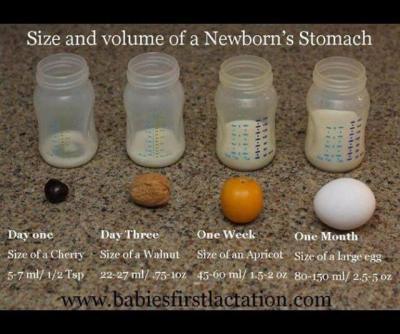
A newborn baby takes in approximately 5-7ml of colostrum per feeding in the first 24 hours. Babies are burning more calories than that as they attempt to breastfeed and expel that sticky, gooey meconium. Nature has provided the perfect amount of colostrum in those first few days to nourish your baby and while the quantity is small, the quality is jam-packed with every calorie, immunological property, protein, vitamin, and laxative that your newborn needs to poop and pee. Babies are expected to lose weight in those first few days. That doesn’t mean that mom’s supply is low.
Babies typically lose weight until mom’s ‘fuller milk’ comes in:
The amount of colostrum continues to grow as your milk transitions to ‘fuller milk’, which comes in around 2-5 days (depending on baby’s access to breast, effective sucking, birth interventions, etc.) Typical colostrum amounts are about 5-7 ml per feeding in first 24 hours, 7-15ml per feeding from 24-48 hours, and 22-27ml per feeding from 48-72 hours. Your baby will most likely lose weight until your ‘fuller milk’ comes in, but that doesn’t necessarily mean that you don’t have enough milk. What parents want to look for is that their baby is peeing and pooping (at least 1 of each per day of life) and baby’s weight loss plateaus once mom’s fuller milk has come in.
Here’s a great graphic of a baby’s stomach from Babies First Lactation and Education
Delayed milk supply doesn’t equal low milk supply:
There are several situations where a mother is at a higher risk for a delayed milk supply. As mentioned in this Best for Babes article, there are a number of factors that increase a mother’s risk for delayed milk supply. Some are beyond our control (or difficult to control): diabetes, obesity, thyroid problems, hypertension, PCOS, preterm birth, and anemia. There are also factors related to birth that can influence when a mother’s fuller supply comes in: cesarean birth, receiving lots of IV fluids, prolonged pushing stage, stress, cascade of interventions, hemorrhaging, mother-baby separation, just to name a few. If you are at a higher risk for having a delayed milk supply, it can be very helpful to speak with a lactation consultant within the first 24 hours after your baby is born. She can teach you ways to hand express and pump to help speed up the process of your fuller milk coming in, thereby DECREASING your risk for a low milk supply.
Lots of fluid during labor can cause greater weight loss in babies:
Studies have shown that mothers who have long periods of birth interventions (epidural, Pitocin, eventual emergency cesarean, etc.), tend to have more fluids during labor, thereby inflating baby’s birth weight and causing a large drop in baby’s weight in the first 24 hours. In those first 24 hours, we are looking for 1 pee and 1 stool (as a minimum.) For those babies that pee and stool multiple times in the first 24 hours, their weight loss is going to be greater, but that is not an indicator that mom’s supply is low. It just means they had a lot of fluids to expel after birth. Here are a few articles that explain this phenomenon. Dr. Jen: Newborn Weight and The Boob Group: Birth Interventions and Their Impact on Breastfeeding.
Baby may lose weight (or gain weight really slowly) because they are having a difficult time transferring mom’s milk:
There are many reasons why a baby might lose weight, sometimes continuing past the first week of life, even when mom has a full supply. Some of these include: engorgement (causing baby to have difficulties latching on), tongue-tie or lip tie, baby is recuperating after a difficult labor, baby is jaundiced, premature baby, etc. Again, when baby is losing weight due to these situations, it doesn’t always mean that mom’s supply is low. If her baby is having a difficult time transferring milk, then she should definitely meet with a lactation consultant to make sure she is doing everything she can to protect her milk supply until her baby can start to efficiently transfer milk from her breast.
Supplementation doesn’t equal formula:
If your milk supply is delayed, if your baby has elevated bilirubin, if your baby has lost more than 10% of his/her birth weight, that doesn’t automatically equal FORMULA supplementation. Mom may actually have enough of her own milk to supplement her baby with until baby’s weight is back on track. All she has to do is hand express or pump and see what extra she has. If mom doesn’t have enough of her own milk to supplement, then the hand expression or pumping (in addition to breastfeeding) will help to bring in her milk supply more fully. In the meantime, moms have other options. A mom can use milk bank breast milk or donor milk, if she prefers. For terrific information about milk banks, check out Human Milk Banking Association of North America and for milk sharing, check out Eats on Feets. The most important take away of this all…. When supplementation is necessary, it is imperative for a mom to increase her breast stimulation to help bring in her supply more fully. When her baby is getting a supplementation from another source, it is saying to mom’s body that she doesn’t have to make that amount of milk, which is totally not the case. The sooner mom’s fuller milk comes in, the sooner supplementation can decrease, so spend the extra time and effort… it will be worth it in the end.
Important note: When you might become concerned about your milk supply
While all of the above statements should illustrate why a mother should not be told that she has a low milk supply early on, there are some situations that might indicate that mom has a low milk supply (either temporarily or more long term.) If you are experiencing any of these situations, please connect with an IBCLC as soon as possible, as sometimes this can be a very temporary situation, as long as measures are taken quickly to protect mom’s milk supply. Here are some indicators that mom’s supply might be low:
Breasts did not grow and/or areola didn’t get darker during pregnancy
Breasts don’t feel heavier or fuller by 5-7 days postpartum
Fuller milk hasn’t ‘come in’ by 5-7 days postpartum
Baby is continuing to need supplementation to gain weight and mom is not making enough to supplement with her own milk
Mom has insufficient glandular tissue
Common Concerns While Breastfeeding: Why are my nipples white?
Are you feeling a burning sensation in your nipples that creeps up into your breasts? Does this happen most often IN BETWEEN feedings, rather than during your breastfeeding session? Have you noticed that your nipples turn white as soon as your baby pulls off?
What you might be dealing with are vasospasms!
Raynaud’s syndrome, or a vasospasm, is a common phenomenon that affects up to 20% of women of childbearing age. It was originally described as affecting the body’s extremities (hands and feet), but now has been described as affecting many other vessels, including the nipples. The symptoms are often confused with thrush, as both cause a burning sensation in the nipples, yet they are completely different from one another.
Thrush is a yeast infection that can be treated with antifungal treatments (see your article Common Concerns While Breastfeeding: Yikes! Why are my nipples burning?). Vasospasms are constrictions of the blood vessels that usually occur as a result of exposure to cold and are not an indication of an infection. Vasospasms will not be resolved with antifungal treatments.
Are you feeling a burning sensation in your nipples that creeps up into your breasts? Does this happen most often IN BETWEEN feedings, rather than during your breastfeeding session? Have you noticed that your nipples turn white as soon as your baby pulls off?
What you might be dealing with are vasospasms!
Raynaud’s syndrome, or a vasospasm, is a common phenomenon that affects up to 20% of women of childbearing age. It was originally described as affecting the body’s extremities (hands and feet), but now has been described as affecting many other vessels, including the nipples. The symptoms are often confused with thrush, as both cause a burning sensation in the nipples, yet they are completely different from one another.
Thrush is a yeast infection that can be treated with antifungal treatments (see your article Common Concerns While Breastfeeding: Yikes! Why are my nipples burning?). Vasospasms are constrictions of the blood vessels that usually occur as a result of exposure to cold and are not an indication of an infection. Vasospasms will not be resolved with antifungal treatments.
What are vasospasms?
Imagine sitting cross-legged and your foot ‘falls asleep.’ Your foot becomes numb as the blood leaves the area. As soon as you start banging your foot on the floor and ‘waking it up,’ the blood flows back into your foot, causing a sensation of pins and needles. This is the same philosophy with nipple vasospasms. Essentially, as soon as your baby’s warm mouth leaves your nipple, the cold air triggers a vasospasm, causing the blood in your nipple to escape and leave the area. This causes blanching, or whiteness of the nipple, since the blood is constricted. Then, as the blood comes back and starts to flow better, the nipple is ‘woken up,’ causing a burning sensation. This can be extremely painful and frustrating, as the throbbing can be felt throughout the entire day and night.
Symptoms for vasospasms:
- Nipples turn white as baby pulls off from feeding (due to the restricted blood flow to the nipples)
- As blood flows back into the nipples, they turn from white to blue, purple, or red, accompanied by throbbing, burning pain.
- Nipples throb in between feedings, especially when mom feels cold or if she feels a let-down, rather than during a feeding.
It is important to rule out the following, as they can also cause vasospasm-like symptoms:
- Poor latch that compresses and/or pinches the nipple
- Tongue-tie
- Sensitivity to nipple creams
- Thrush/breast infections
- Pregnancy
*** None of these can be treated with vasospasm remedies
Once you have ruled out other causes of vasospasms, you can begin to treat them.
How to treat vasospasms:
- Avoid vaso-constricting substances, such as nicotine, caffeine, and alcohol
- Try to keep your nipples and breasts warm in between feedings. Wool breast pads, such as the ones made by LanaCare, can be fantastic
- Try herbal and vitamin supplements to help increase blood flow and reduce symptoms. My favorite daily regiment is 5000IUs of vitamin D3, 200mg of vitamin B6, the minimum dosage of Natural Calm Magnesium, and Nordic Naturals Omega 3 vitamins.
- Acupuncture – since vasospasms are caused by lack of blood flow to the nipples, acupuncture can help move your blood and keep it from being stagnant in your body
- If none of these measures help with the pain, speak with your doctor about nifedipine, a calcium channel blocker that has vasodilatory effects. Nifedipine, as any medication, has risks of side-effects. These side effects include dizziness, headache, and tachycardia, so please consult your primary healthcare provider.
As always, it can be very helpful to meet with an IBCLC to determine whether your nipple pain is due to vasospasms or to another breastfeeding issue. You can find an IBCLC in your area on the International Lactation Consultant Association website.
Common Concerns While Breastfeeding - Yikes! Why Are My Nipples Burning?
Welcome to our blog series…. Common Concerns While Breastfeeding. These aren’t the complicated, ‘come-to-my-house-immediately’ phone calls I receive. Rather, these are the questions that come from clients and friends in the middle of the night, by text or by email, that don’t necessarily warrant a lactation consultation. They can often be easily resolved with a few simple tricks. So, I would like to share those tricks with you!
Why Are My Nipples Burning????
Welcome to our blog series…. Common Concerns While Breastfeeding. These aren’t the complicated, ‘come-to-my-house-immediately’ phone calls I receive. Rather, these are the questions that come from clients and friends in the middle of the night, by text or by email, that don’t necessarily warrant a lactation consultation. They can often be easily resolved with a few simple tricks. So, I would like to share those tricks with you!
Why Are My Nipples Burning????
Oh, those itching and burning nipples and breasts. It takes all of your will power to not walk up to the closest tree and rub your front side on it, like a bear would rub on a tree to get rid of fleas. The itching can feel insatiable. This is often your first sign that you have thrush, which is a yeast infection of a mucus membrane, your breasts being one of them.
How did I get thrush?
Well, just like a vaginal yeast infection, thrush is caused by an overgrowth of yeast in your gut. Breastfeeding moms may often find that they get thrush after a dose of antibiotics. This is because antibiotics kill NOT ONLY the bad bacteria in your gut, but also the good bacteria. Yeast loves when there is an absence of good bacteria in your gut, so it decides to multiply and aim for any mucus membrane.
Moms and babies who also have inflammation, such as a food intolerance which limits the absorption of important nutrients, or are just temporarily dealing with a compromised immune system, are also more susceptible to thrush.
What does thrush look like?
Burning, itchy nipples and breasts
Red or pink nipples and areola
Painful feedings after a time period of painless feedings
And thrush doesn’t just affect the mom.... babies can get thrush as well. When your baby has thrush, he may have white, cauliflower-textured spots in his mouth along the gum line or on his cheeks. He may also have a raging diaper rash. Babies with thrush may cry while breastfeeding because the milk stings the sores in their mouths. And to complicate matters more, your baby may show no signs of thrush at all!
How does one get rid of thrush?
First and foremost, make sure that the pain you are feeling is not due to a less-than-perfect latch. Also, if the burning happens to only occur after the feeding, not during the feeding, it might be worth it to see if you have Raynaud's, which is a vasospasm of the nipple.
Remove sugars (including most fruit and fruit juices) from your diet for about a week. Yeast grows on sugar, so removing it from your diet restricts yeast growth. It might help to eliminate dairy as well.
Consider starting a course of a high-quality probiotics to help recolonize your gut, and your baby’s gut, with good bacteria. I would recommend choosing a probiotic from the refrigerator in the herb section of a natural food store. Probiotics are alive and begin to die off when at room temperature, so don’t purchase anything sitting on a shelf, unrefrigerated.
You will want to wash all of your bras and underwear in a distilled white vinegar rinse cycle. Also, soak anything that goes in the baby’s mouth, like a bottle nipple, in apple cider vinegar before rinsing it in soapy water. The vinegar should help kill off the yeast hanging out on these items.
All Purpose Nipple Ointment (APNO) - if that pesky thrush will not go away after trying the above recommendations, Jack Newman has a protocol for getting rid of thrush. You can ask your primary care physician for a prescription for this to bring to a compounding pharmacy. Midwives often have recipes for this as well, that you can make with over-the-counter medications.
If all else fails, you can ask your physician for Diflucan, which is the same medication used to clear vaginal yeast infections.
Lastly, definitely discuss this issue with your pediatrician or a lactation consultant. He or she may have some other recommendations to help remedy the out of control yeast.
Help a Mama Out: Surviving the First Few Weeks of Breastfeeding
What tips do you have for surviving the first few weeks of breastfeeding?
Maren: Lots of skin to skin to get those endorphins going so you can take advantage of all that delicious oxytocin (which will make you want to keep breastfeeding, even with things might be tough!) Take advantage of all of the support you can – it will help normalize the experience so that you feel totally confident in your decision to breastfeed. And know ahead of time that there is definitely a learning curve, but it only gets better and better, so hang in there!
Amanda: Make sure to talk to your partner about how you need him/her to support breastfeeding and encourage you, even when you get discouraged and feel like giving up!
Jamie: Get the latch correct right away! Take advantage of the lactation consultants at the hospital and ask for a referral even if you don’t think you will need one.
Andrea: Trust your body! Skin to skin, lots of water, and lots of rest.
Heather: Surround yourself with at least one supportive person. I would never have made it through those weeks without the support of my husband.
Alicia: Hire a postpartum doula.
Juli: Surround yourself with women (and men!) who support breastfeeding. It gets easier – it is definitely worth pushing through the tough parts in the beginning!
Billie: Make really good friends with the lactation consultant and local breastfeeding support group before delivery. They will be able to offer so much support in those first few weeks. Trust your supply. Make sure you are comfortable!
Monica: I went to classes and read books, which helped, but nothing prepares you for the real thing. Get help early, if you need it. Hiring a lactation consultant was the best thing I did. Keep telling yourself you will try it for one more day and one day it will become second nature. Coconut oil worked wonders on sore nipples.
Christine: OMG… best advice I got was to rub breastmilk around your nipples after every nursing session! My cracked tatas healed within 2 days of doing that!
Chelle: If it hurts and you are dreading the next nursing session, don’t just tough it out! Get help ASAP before it gets worse or turns into an issue that makes you quit! Take a prenatal class. Breastfeeding is natural, but that doesn’t mean you will naturally know what to do.
Sarah: Don’t expect anything else from yourself. Set up what you can ahead of time and find someone else to do everything else that needs to be done. Establishing your breastfeeding relationship is your job.
Jen: Get a Netflix subscription and ignore the dirty dishes!
Danielle: Don’t do anything but rest, breastfeed, nap, and eat. Nothing else matters right now.
Abbey: Celebrate every success, no matter how small it seems!
Desiree: Find support! And be patient…it’s not always easy, but it’s most certainly worth it!
Sofia: Learn the basics! Before birth is possible! Proper latch, how milk supply works, most common myths about breastfeeding, how to know if your baby is getting enough, why it is REALLY important to feed on cue rather than a schedule, why baby doesn’t need ANYTHING else but your breastmilk, etc.
Amanda: Don’t give up! Get help and support! Spend as much time as you can with your baby (in bed if you can.)
Priscilla: Relax. Don’t listen to anyone that’s not helpful. Determine your own needs for comfort.
Joanna: Expect to care for your baby and get others to help with meals and housework.
Thanks to everyone who responded to our questions on our San Diego Breastfeeding Center and The Boob Group Facebook pages. Check back every Tuesday for a new Help a Mama Out tip!
To find an international board certified lactation consultant, visit www.ilca.org
Here are a few more articles on our website, specifically dealing with breastfeeding a newborn:
Advice for a Newly Breastfeeding Mama’s Partner
Breastfeeding Expectations for the First Month
Newborn Hands: Why are they always in the way while breastfeeding?
Supplement Options: Donor Breastmilk, Milk Banks, and Formula
This past week, we released one of my most favorite episodes on The Boob Group: Low Milk Supply: Donor Milk, Milk Banks, and Formula. I had the esteemed pleasure of interviewing Amber McCann, an International Board Certified Lactation Consultant, fierce supporter of all things mothering, and dear friend. I wanted to know what options were out there for mothers who needed to supplement their babies, as well as the pros and cons of each.
I pulled out the most salient points for this blog article, but you can click here to listen to the Boob Group episode in its entirety: Low Milk Supply: Donor Milk, Milk Banks, and Formula.
What are your options if you need to supplement your baby?
When feeding an infant, the World Health Organization lists a hierarchy:
- Milk taken directly from the mother’s breast
- Expressed milk from baby’s mother
- Expressed milk from another mother (wet nurse, donor milk, milk from a milk bank, etc.)
- Breastmilk substitute (formula)
This past week, we released one of my most favorite episodes on The Boob Group: Low Milk Supply: Donor Milk, Milk Banks, and Formula. I had the esteemed pleasure of interviewing Amber McCann, an International Board Certified Lactation Consultant, fierce supporter of all things mothering, and dear friend. I wanted to know what options were out there for mothers who needed to supplement their babies, as well as the pros and cons of each.
I pulled out the most salient points for this blog article, but you can click here to listen to the Boob Group episode in its entirety: Low Milk Supply: Donor Milk, Milk Banks, and Formula.
What are your options if you need to supplement your baby?
When feeding an infant, the World Health Organization lists a hierarchy:
- Milk taken directly from the mother’s breast
- Expressed milk from baby’s mother
- Expressed milk from another mother (wet nurse, donor milk, milk from a milk bank, etc.)
- Breastmilk substitute (formula)
Is it safe to offer your baby another woman’s breastmilk?
Making the decision as to what to feed your baby should never be taken lightly. It is important when one is considering offering donor breastmilk to their baby to balance the risks and benefits. You should always consider asking the potential donor mom for a copy of her prenatal blood work to check for sexually transmitted diseases and other potential pathogens. It is also important to ask questions about lifestyle choices, such as alcohol use, smoking, diet, medication use, etc. Eats on Feets has a Resource Guide with great lists of questions for both the donor and recipient of expressed breastmilk, as well as an extensive list of health considerations.
What are the main benefits of using donor milk?
- It’s breastmilk! It has everything your baby needs, nutritionally and immunologically.
- It has every benefit that a mother’s own milk would have.
What concerns may arise when using donor milk?
- A number of pathogens enter into human milk if a mother is infected, however few diseases can be transmitted through human milk, itself.
- The main diseases that cause concerns are HTLV, HIV, and CMV. CMV is typically only a challenge for premature infants. Fortunately, HTLV can be deactivated by freezing and HIV by flash heating.
Where can a mother find someone to donate milk?
- Start with your own social group. If you have friends or friend of friends who are breastfeeding, there is always a chance that they or someone they know has an excess supply in their freezer or would be willing to pump for you, if they knew there was a need. All you have to do is ask!
- Informal milk groups, such as Eats on Feets and Human Milk for Human Babies
- Milk Banks
What are milk banks?
Milk banks are non-profit organizations where breastfeeding moms can donate breastmilk, should they fit the milk bank’s criteria. The Human Milk Banking Association of North America requires that their donors be in good health, not regularly on most medications or herbal supplements, willing to undergo additional blood testing, and be willing to donate at least 100 oz. Donated human milk is pasteurized and then either sold to hospitals to feed critically ill babies or to families who purchase directly from the milk bank.
How should I choose between donor milk, milk from a milk bank, or formula?
This is such a hard decision and definitely not one to take lightly! What is most important is to look at your needs, your baby’s needs, what you feel most comfortable supplementing with, and what’s the best choice for your family. So, sit down, research all of your options, and choose with your heart and knowledge.
As a follow up to this article, several moms submitted stories about their experiences using donor milk or donating to a friend or milk bank. Stay tuned, as we share them during the rest of the week!
If you have a story about using donor milk or donating breastmilk to a friend or milk bank, and you want to share it with our readers, please email it to me at robinkaplan@sdbfc.com.
Did you have to supplement your baby with donor milk, milk from a milk bank, or formula?
How did you choose which supplement to use?
Update on 2013-01-24 15:36 by Robin
Here's your Call to Action:
Too many breastfeeding mothers have no idea that human milk sharing is an option and we want to change that!
If you are a breastfeeding mother and have used donor milk or have donated your own milk, we would love to hear your story! Other breastfeeding moms need your support! Just knowing that someone else out there went through a similar experience.... well, that can make all of the difference in how a mother views her own breastfeeding experience! Your stories are beyond powerful! They need to be heard!
If you would like to have your stories posted on our website, as well as The Boob Group's website, please send your story to robinkaplan@sdbfc.com.
We will begin posting your stories as soon as we receive them!
Toddler Nursing Part III - Super Breastfed Baby!
Written by guest blogger, Andrea J. Blanco, IBCLC
My seven year old is really, really into the Super Diaper Baby series. So much so (embarrassing story for which I will pay for dearly in 10 years coming up right now) that the other day, he fished through all the dirty clothes to find 8 (yes, 8!!!!) underwear to put on simultaneously along with a cape so that he could reenact parts of the book. I’m not entirely sure why clean underwear couldn’t be used, but hey, welcome to the gnarly world of 7 year old boys. I’m still getting adjusted. Anyway, whenever he yells “SUPER DIAPER BABY!!” all I hear is “SUPER BREASTFED BABY!!!” (you better have read that in your booming announcer voice; if not, please go back and reread).
Written by guest blogger, Andrea J. Blanco, IBCLC
My seven year old is really, really into the Super Diaper Baby series. So much so (embarrassing story for which I will pay for dearly in 10 years coming up right now) that the other day, he fished through all the dirty clothes to find 8 (yes, 8!!!!) underwear to put on simultaneously along with a cape so that he could reenact parts of the book. I’m not entirely sure why clean underwear couldn’t be used, but hey, welcome to the gnarly world of 7 year old boys. I’m still getting adjusted. Anyway, whenever he yells “SUPER DIAPER BABY!!” all I hear is “SUPER BREASTFED BABY!!!” (you better have read that in your booming announcer voice; if not, please go back and reread).
Super Breastfed Baby is not a baby anymore. He’s a toddler who can leap off everything, get all bruised up and bounce right back up. He can run amazing distances while laughing hysterically at you chasing him and fall over 15 times, but who’s counting? He scoffs at the mere thought of you trying to clean. Or sit. Or cook. Or sleep. He knows what he wants and isn’t taking no for an answer. This is the breastfed baby magnified – the one that I was reminded of as I read some of your comments to Toddler Nursing Part I and Toddler Nursing Part II of the Toddler series. Super Breastfed Baby is who we’re going to tackle today.
The Scenario: You and Super Breastfed Baby are home and you are trying to get things done around the house.
I hate to say it, but nothing about this will ever get easy. But it can get easier. Having a child, nursing or otherwise, around the house means being very strategic in all that you do. Your toddler wakes at 7, you say? Well then, 6:15 is the time to set the alarm so you can chop veggies for tonight’s dinner, put a load of laundry in the washer, and prepare a to-do list for your partner. Waking earlier than your little one doesn’t work for you? Try naptime or after bedtime. When they’re awake what they want is to be entertained. By you. Because you’re the awesomest. EVER. And no one else can compare to the way YOU entertain them. And when you aren’t in the entertaining mood? You still have breasts. Which they love. All I keep thinking as I’m typing this paragraph is “That which you resist, persists.”
It’s easy to get caught up feeling like “I HAVE TO DO THIS NOW”, but sometimes, if you stop for a second and give in to Super Breastfed Baby’s demands (of nursing or block building or nursing while block building), you will find that time to do what you were looking to do suddenly appears afterwards. And if it doesn’t appear? And you still have to vacuum? Rip a play out of my dear friend’s book and wear your baby right around naptime. She vacuums the floors, makes the bed, washes the dishes and sometimes even mows the lawn with her toddler strapped to her back in the Ergo. Most times he’s too busy loving the view, but sometimes, her little superhero falls asleep while she’s at it.
The Scenario: You and Super Breastfed Baby are, well, just home.
You may have noticed that when you’re home or *gasp* sitting down, your normally easy to distract child becomes Mr. Grabby Pants (which definitely feels like a superhero quality), demanding to nurse every. five. minutes. This one is a little trickier to fend off because mommy sitting = easy target. Most toddlers nurse that frequently out of boredom and/or familiarity. If you’re like most moms, for the last year, most of you and your baby’s breastfeeding took place either sitting or laying down. So it just means that your little princess was paying attention and now that she sees you sitting or laying down again, she thinks it’s nursing time. If you have realistic expectations of what’s about to happen, then you may be better prepared to deal with it. Another way to fend off Mr. or Ms. Grabby Pants is to “relax” in a new or exciting (but safe) environment. Toddler areas at local museums or indoor play gyms tend to be enclosed – use that to your advantage. Your busy, curious, newly independent toddler will be much less likely to think of nursing when there’s other stuff to do and see.
The Scenario: You and Super Breastfed Baby are at an impasse and you’re not too sure you want to continue nursing.
You’re trying to set boundaries, but it seems nothing is working. It’s not so much that you want to wean Super Breastfed Baby (or maybe it is), but you would like for nursing to feel like it’s more on your terms than at his demand. First, there is absolutely NOTHING wrong with you feeling that way. Nursing is a mutual relationship – both you and your child have to want to continue. As I mentioned in Part II, if you’re feeling like you want to slow down the demands of nursing or even wean, first try to pinpoint which is the MOST difficult nursing time for you. For me, it wasn’t the morning, nap and night – those I could deal with. But it was all the in-betweens. However, I didn’t realize that I could deal with, and actually cherished, the morning, nap and night until I was able to really cut back on the in-betweens. It took lots of creativity and motion, but after a few weeks, he didn’t even realize the in-betweens were missing. As with any change to a child’s sense of normalcy, employing gentle techniques combined with lots of love and patience along with waiting (if you can) until the child is communicative enough to understand, even if he doesn’t agree, will yield the best results.
The Scenario: You and Super Breastfed Baby have found your groove, but sometimes, she acts like there isn’t enough milk.
Super Breastfed Baby is one smart cookie. Maybe it’s that x-ray vision or her supernatural senses, but something has alerted her that there is less milk. Did you read that sweet momma? LESS MILK. Less milk is different than “NOT ENOUGH” milk. A few months ago, when you started solids because your little one showed all the signs of being ready, the weaning process began. Your body naturally slowed down its milk production to meet your baby’s needs and has continued to be super efficient in adjusting to those continued needs. Yes, you do have less milk, but, in conjunction with the other foods he’s eating, he’s still getting exactly what he needs. In addition, Super Breastfed Baby knows what he’s doing when he seems to be kneading the breast or trying to “play” with the other nipple. He’s actually trying to elicit a faster flow of milk for himself. For most moms, the kneading is nowhere near as exasperating as the nipple twiddling. Toddlers need to learn manners, too, and where better to learn them then at the breast where they are happy and relaxed and met with love? If you’re trying to curb behaviors such as nipple twiddling, be consistent each time. Explain to your toddler that it hurts momma. Use words she can understand. And repeat each and every time. Sometimes, along with consistency, a little bargaining might help, too. “Instead of hurting mommy by touching my breast that way, you can [insert substitutive, less exasperating behavior here]”.
So many of my past New Year’s Eves were spent with a baby in arms, or in a sling, or on the breast, picking confetti (or food) out of their beautiful, thick brown hair. Some years, it seemed I would never have my body free at midnight – or ever. My Super Breastfed Babies are babies no more…I can’t even say they are in jest. This year, we weren’t nursing at midnight. I wasn’t holding them. Yet, there we were, all of us snuggled up and interlocked when the clock struck 12. Maybe not as it had been in years past, but then again, not much different either. Maybe it was because, as others would say, I “nursed them *forever*”. Or maybe it’s because, through the nursing process, I realized there’s nowhere else I’d rather be.
Happy New Year!
Andrea Blanco is an International Board Certified Lactation Consultant at The Milk Collective Lactation Care, working with families in the Miami/Ft. Lauderdale area. She is the proud mom of 2 loving, spirited boys, who teach her humility, patience, humor, and the rules to more sports than she thought she’d need to know every day. When she’s not helping families achieve their breastfeeding goals, you can find her on the sidelines, at karate tournaments, or with her toes in the sand. She can also be found at themilkcollective.co, on Instagram @themilkcollective_ , facebook.com/themilkcollectivelactation or by email at: andrea@themilkcollective.co.
Do you have any additional questions for Andrea about nursing a toddler? Share them in the comment section and we'll ask her to write another article!