Nurturing your Child's Potential with Voila Montessori
This week, we’re highlighting a local practitioner who is helping parents establish and integrate their parenting beliefs and styles into a peaceful, nurturing environment for their children. She also offers Skype consultations for those not located in San Diego. I’m thrilled to introduce Jeanne-Marie of Voila Montessori!
This week, we’re highlighting a local practitioner who is helping parents establish and integrate their parenting beliefs and styles into a peaceful, nurturing environment for their children. She also offers Skype consultations for those not located in San Diego. I’m thrilled to introduce Jeanne-Marie of Voila Montessori!
_____
1. What does it mean to have a Montessori home?
A Montessori home is one that is adapted to meet the child’s ever changing needs, as well as it being nurturing, peaceful and respectful to all family members. It is a home where obstacles to children’s natural development are minimized, enabling children to become life long independent and confident learners.
2. What modifications do you help parents make in their homes? Why are these modifications important?
When helping parents make simple adjustment, I first look at the four main areas depending on the child’s age and the size of the home. These areas are the sleeping, feeding, personal care and movement areas. For example the feeding area at first will be for the sole purpose of bonding with the child while breastfeeding. I usually recommend a quiet, comfortable place where the caregiver can give a 100% of their attention to the infant. This area will then change once the child is introduced to other foods.
To name only a few simple ideas I share with parents: make sure children have access to real child-size utensils to do ‘real work’, such as cooking, cleaning, personal care, caring for animals or plants as well as creating a quiet reading area just for them etc. I also recommend many different activities to set-up depending on the age and interest of the child.
(photo credit: Laura Christin Photography)
These modifications evolve and change as the child grows and their needs are different; they are not going to be the same for an infant as they are for a walking toddler or a preschooler. These changes are also about being mindful parents, aware of the child’s needs by learning to observe and never interrupting when they are concentrating on their own self-construction.
I believe that these changes are important in that they help the entire family to live in peaceful harmony. These are small modifications that will make a world of difference for everyone involved. They are wonderful tools for the development of the child’s will as well as their self-esteem “I can do it!”
3. How does clutter in the home affect a child's ability to reach his/her full potential?
Clutter is actually an obstacle to their development. A home that is cluttered with too many toys and activities can be very overwhelming for a young child. Children have a real need for order and routines in their early years. External order brings internal order. Young children are absorbing so much information in these early years that it is helpful for the home to be clutter free and orderly to help them make sense of it all. I am always overjoyed to hear parents tell me how much their child’s behavior improved by simplifying their play area.
4. How does having a Montessori home go hand in hand with Positive Discipline?
Beautifully! There are a lot of misconceptions about Montessori that it is a place “where children are left to do whatever and it is a free for all”. Montessori is actually a very simple and intuitive way of life and educational method, where all freedoms are within limits. Positive Discipline is a great compliment to Montessori since it is a very respectful way of guiding children. It is firm and kind at the same time believing that connection before correction is crucial for the child’s healthy development.
5. What type of consultations and classes do you offer to local parents? Do you conduct Skype visits?
I have many different types of consultations. I work with expectant parents helping set-up a baby-focused nursery as well as parents, grandparents and any caregivers of young children from birth to six years. My consultations are for families wanting guidance on how to adapt their home to meet their child’s needs as well as for families who need help with having children be more cooperative and respectful.
I offer workshops throughout the San Diego County. Small workshops can be created for specific parent groups.
I am also available to help set-up larger learning environments such as home daycares or family home school co-ops.
Yes, I do offer long-distance consultations either by phone or via Skype. Parents from different parts of the country and world have asked for advice, so I needed to make myself available. I’m also working on developing some online webinars.
_____
Jeanne-Marie's multicultural upbringing and travels planted the seeds of a lifelong curiosity regarding the fundamental needs of children and families.
Her goal is to help parents appreciate the true importance of their role – not as servants or teachers, but as supporters and guides of their children’s natural development. Families who work with Jeanne-Marie reap the benefit of her Masters in Montessori education, her two AMI Montessori certifications covering childhood development from birth through age 6, her Positive Discipline certification for both parents and the classroom as well as her extensive classroom experience, and first-hand parenting knowledge.
She launched Voila Montessori in response to the overwhelming demand from parents for advice and guidance for raising children in a gentle, peaceful, and supportive environment that’s conducive to their full development – psychological, academic, artistic, spiritual, physical, cultural, etc.
Jeanne-Marie describes herself as “genuine, passionate, and straightforward”. She’s honest and direct, because she realizes that clear and precise information is what will help parents cut through the overwhelming amount of advice that engulfs them.
To learn more about Jeanne-Marie and how she can support you and your children, please visit www.VoilaMontessori.com and like her page, Voila Montessori, on Facebook.
Jeanne-Marie will be offering a monthly workshop at Nature’s Whisper Yoga starting Thursday, November 21, 2013.
Breastfeeding for the Adoptive or Intended Mother
Last week I had the pleasure of speaking at a workshop for families considering adoption and/or surrogacy. The topic of my presentation was Breastfeeding for the Adoptive or Intended (through surrogacy) Mother. Most of the families in the audience had no idea that a woman could breastfeed without birthing her child and their faces just lit up when I discussed that this was a possibilty for them.
While I have worked with several mothers in San Diego to induce lactation for an adopted baby or baby born by surrogate, I thought I would invite my colleague, Alyssa Schnell, to answer a few questions about this process. Not only has Alyssa personally experienced inducing lactation for her adopted daughter, but she also recently published a book on this topic as well, titled Breastfeeding Without Birthing: A Breastfeeding Guide for Mothers Through Adoption, Surrogacy, and Other Special Circumstances (Praeclarus Press, 2013)
Last week I had the pleasure of speaking at a workshop for families considering adoption and/or surrogacy. The topic of my presentation was Breastfeeding for the Adoptive or Intended (through surrogacy) Mother. Most of the families in the audience had no idea that a woman could breastfeed without birthing her child and their faces just lit up when I discussed that this was a possibilty for them.
While I have worked with several mothers in San Diego to induce lactation for an adopted baby or baby born by surrogate, I thought I would invite my colleague, Alyssa Schnell, to answer a few questions about this process. Not only has Alyssa personally experienced inducing lactation for her adopted daughter, but she also recently published a book on this topic as well, titled Breastfeeding Without Birthing: A Breastfeeding Guide for Mothers Through Adoption, Surrogacy, and Other Special Circumstances (Praeclarus Press, 2013)
_____
Why would a mother consider breastfeeding her adopted baby or baby born by surrogate?
Most people are not even aware that it is possible to breastfeed a baby who arrives via adoption or surrogacy! The lucky few adoptive or intended (through surrogacy) mothers who learn that breastfeeding is possible for them usually learn about it through their own diligent research. Many times, breastfeeding is just a sentence or two in a book about adoption.
What are some benefits of breastfeeding an adopted baby or baby born by surrogate?
Breastfeeding is the normal, healthy way to feed and nurture babies. All babies. And babies who arrive via adoption or surrogacy may benefit from breastfeeding even more than most babies.
- Human milk protects babies against illness. The protection can be especially important for babies who have experienced adoption since adopted babies - for several reasons - are more likely than other babies to get sick (Gribble, 2006).
- Breastfeeding helps babies attach to their adoptive or intended mothers. All babies who experience adoption or surrogacy experience a disruption in attachment, because babies begin attaching to their mother in utero (Gribble, 2006). Some adopted babies experience multiple breaks in attachment if they are in foster or institutionalized care before adoption.
- Breastfeeding helps babies to develop normally. Babies who experience adoption are more likely to be developmentally delayed due to drug or alcohol exposure in utero, parental abuse, and/or institutionalized care.
Are there benefits for the mother, as well?
Yes, breastfeeding is just as important for mothers as it is for babies. And, just as with babies, adoptive and intended mothers may benefit from breastfeeding even more than other mothers.
- Breastfeeding is a normal part of the female life cycle. It provides protection against breast, ovarian, and uterine cancers, osteoporosis, and cardio-vascular diseases. For women who do not experience the health benefits of pregnancy, breastfeeding can be especially important (Ip et al., 2007; Collaborative Group on Hormonal Factors in Breast Cancer, 2002).
- Breastfeeding can help heal the loss associated with infertility. Breastfeeding provides a unique opportunity for the adoptive or intended mother to participate in her baby’s birth cycle.
Can a mother breastfeed without making milk?
Yes! A mother can most definitely breastfeed without making milk. She can feed her baby at her breast using an at-breast supplementer (a feeding tube attached to the breast) such as a Lact-Aid or Supplemental Nursing System (SNS). Or, she can bottle-feed her baby and comfort nurse her baby at the breast (just as a baby might suckle on a pacifier for comfort). Breastfeeding is so much more than making milk!
Photo credit: Barbara Robertson, IBCLC
If a mother wanted to make milk for her adopted baby or baby born by surrogate, what are her options?
Even without being pregnant, frequent stimulation of the breasts and nipples - usually by a nursing baby or an electric breast pump - can cause a woman’s breasts to start making milk. Taking medications or herbs can help the breasts to start making milk sooner and/or more abundantly. Most mothers who induce lactation, or make milk without pregnancy and birth, will produce some milk and a few will produce a full milk supply. Many adoptive or intended mothers will use an at-breast supplementer so that they can fully feed at the breast even if they are not producing a full milk supply.
Several protocols, or step-by-step instructions, have been developed to help adoptive or intended mothers induce lactation. In my book Breastfeeding Without Birthing, I describe five protocols for inducing lactation, ranging from very simple to more intricate. The simplest protocol for inducing lactation has been used by adoptive mothers in developing countries where there is no access to breast pumps or medications for inducing lactation. Another protocol uses an electric breast pump and herbs but no pharmaceutical medications. Another uses an electric breast pump as well as a couple of pharmaceutical medications. Each adoptive and intended mother is encouraged to choose a protocol that suits her individual values and circumstances or, with the guidance of an International Board Certified Lactation Consultant, to mix-and-match the established protocols in order to customize an approach just right for her.
An adoptive or intended mother can start the process of inducing lactation, or making milk without pregnancy and birth, several months or weeks before her baby arrives. She can also wait until her baby is in her arms to begin. There really isn’t one ideal time to start inducing lactation, since each mother’s circumstances are unique.
_____
About Alyssa:
I am an International Board Certified Lactation Consultant (IBCLC) in private practice, a La Leche League Leader, and mother to three breastfed children – two by birth and one by adoption. Breastfeeding my adopted daughter was a highlight of my life – something so special and so important to both of us that I want to do whatever I can to help other adoptive or intended mothers and their babies have the same opportunity we did. For more information on breastfeeding a baby arriving by adoption or surrogacy, see my new book Breastfeeding Without Birthing: A Breastfeeding Guide for Mothers Through Adoption, Surrogacy, and Other Special Circumstances (Praeclarus Press, 2013). It is available through my website www.BreastfeedingWithoutBirthing.com or on Amazon. My facebook page is another great way to keep in touch! www.facebook.com/BreastfeedingWithoutBirthing .
References:
Collaborative Group on Hormonal Factors in Breast Cancer. (2002). Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease. Lancet, 187-195.
Gribble, K. (2006). Mental health, attachment and breastfeeding: implications for adopted children and their mothers. International Breastfeeding Journal, 1(5). doi:10.1186/1746-4358-1-5
Ip et al. (2007). Breastfeeding and maternal and infant health outcomes in developed countries: evidence report/technology assessment no. 157. Rockville, MD: Agency for Healthcare Research and Quality.
Breastfeeding in the Operating Room
Over the next few weeks we will be sharing stories of triumphant breastfeeding mamas and their biggest supporters who helped them reach their personal breastfeeding goals.
_____
This story is from Dawn.
I have to thank my hospital TEAM for my breastfeeding success!
When I gave birth to my son 5+ years ago, it wasn’t what any first time mom would like to experience. I was having problems with maintaining my blood pressure and when my little boys’ heart rate dropped too low, I was rushed into an emergency c-section. It was an extremely frightening process that didn’t even enter my mind as a possibility. The months that followed were hard. We struggled at finding a proper latch and feeding became such a difficult task, I dreaded it.
It never occurred to me that our difficulties at latching could have been because of the birth experience .
Over the next few weeks we will be sharing stories of triumphant breastfeeding mamas and their biggest supporters who helped them reach their personal breastfeeding goals.
_____
This story is from Dawn.
I have to thank my hospital TEAM for my breastfeeding success!
When I gave birth to my son 5+ years ago, it wasn’t what any first time mom would like to experience. I was having problems with maintaining my blood pressure and when my little boys’ heart rate dropped too low, I was rushed into an emergency c-section. It was an extremely frightening process that didn’t even enter my mind as a possibility. The months that followed were hard. We struggled at finding a proper latch and feeding became such a difficult task, I dreaded it.
It never occurred to me that our difficulties at latching could have been because of the birth experience.
In early 2012 we received good news, we were expecting! I did my best to set everything up for a different birthing experience. I searched out a CDC accredited Baby Friendly Hospital in my area, researched VBAC’s and educated myself on the benefits of skin-to-skin. It wasn’t until closer to my due date that I was informed I couldn’t have a VBAC. No hospital would even consider me as a potential VBAC candidate because of my small heart issue as well as my age. After fighting and pleading, I had to acknowledge that I had no other option, but another C-section.
I may have lost that battle, but I was going to do everything in my power to have skin-to-skin with my little girl. I was aware of the evidence-based research on the benefits of skin-to-skin and its success rate with c-section births. I talked to my pediatrician about this and he agreed. (I since found out that it is the pediatrician who is in charge in the OR!) I wrote my birth plan with the intentions of doing skin-to-skin immediately after the c-section unless there was a medical reason not to.
Alas, I wasn’t able to make it all the way to my scheduled c-section date. This time I was low on amino fluids and baby’s lack of movement put me into the hospital at 36 weeks. With concern, my OB and the pediatrician, agreed, that under supervision, they would monitor me and try to get us to the 37th week and do the c-section.
Now, prior to this, we made sure to talk with all the right people about our wishes for skin-to-skin. Everyone was on board: our OB, the hospital’s labor and delivery nurses, and staff. In fact, the hospital staff has been championing the change in procedures to allow skin-to-skin in the OR without success.
The day of my C-section, my regular pediatrician was out of town and his standing replacement wasn’t comfortable at all. I had to conveince the standing pediatrician that this was in my and my baby's best interest. The hospital's Head Labor & Delivery nurse helped us get to a compromise! She is my angel! She proposed that if everything looked good my little girl would be immediately placed on my chest, without ANY other intrusion.... meaning the vernix would be wiped off her while she was on my chest and she would be weighted and measured later.
When the hour came for us to have the c-section more drama around skin-to-skin unfolded, this time all the way up to the director of the Family Birth Center. The director of the Family Birth Center was completely opposed to it and tried talking my OB out of it. We were lucky we had enough support and commitment from the labor and delivery nurses and my OB to move forward. We finally got our wish!
I have to admit, because she was coming 3 weeks early, I wasn’t sure we would even get the option of skin-to-skin, but our little girl emerged perfectly! She was screaming and quickly confirmed in perfect health!
When she was placed on my chest and covered with a warming blanket, I was in awe. This little 6 pound bundle was just perfect. After a little while, she actually scooted and rooted for my breasts and eventually latched and nursed! I just didn’t think I would get that experience since she was early. The remembrance still makes me cry. It was such an amazing experience. I was so happy I had the team in my corner and the hospital went forward with my wishes.
When I was first told I would have to have another cesarean, I felt completely out of control and very disappointed. Creating a birth plan around my c-section allowed me to take a bit of control back and talking with all parties that come with a c-section allowed me the skin-to-skin connection that was deeply important to me.
It has been over a year since Beth was born. We are still nursing strong and have a connection that I attribute to the wonderful team that helped me get skin-to-skin in the OR!
Side note: I have since heard that they have allowed other moms the same experience! The hospital team not only helped me, but also have persevered in getting policy “changed” at the hospital!
Dawn Alva
Comebacks for ‘Why Are You Still Breastfeeding?’
Any woman who has ever had a breastfeeding challenge or has breastfed longer than than someone else deems ‘normal’ has been asked this question at one time or another.
“Why are you still breastfeeding?”
Sometimes this question is passive aggressive with undertones of “I can’t believe you have breastfed your baby for THIS long.” Other times it comes from a place of love meaning “You seem like you are in pain... are you sure you still want to try this?”
Regardless, if you are anything like me, the snappy comeback or educated response that I SO desired to say only comes after the situation is long gone and I am kicking myself for not defending myself and my choice to breastfeed the way I wanted to.
Any woman who has ever had a breastfeeding challenge or has breastfed longer than than someone else deems ‘normal’ has been asked this question at one time or another.
“Why are you still breastfeeding?”
Sometimes this question is passive aggressive with undertones of “I can’t believe you have breastfed your baby for THIS long.” Other times it comes from a place of love meaning “You seem like you are in pain... are you sure you still want to try this?”
Regardless, if you are anything like me, the snappy comeback or educated response that I SO desired to say only comes after the situation is long gone and I am kicking myself for not defending myself and my choice to breastfeed the way I wanted to.
Well, ladies... look no further!
Here are some handy, snappy (evidence-based) comebacks that you can tuck away in your back pocket, only to whip out at the most appropriate times, pun intended! (P.S. These comebacks also work if someone asks why you are STILL exclusively pumping!)
Top 10 Comebacks to Answer the Question: Why Are You Still Breastfeeding?
1. “It’s the perfect food for my child. 24 hours a day, 7 days a week!”
- Babies can digest human milk more easily than the milk of other animals, probably because human milk contains an enzyme that aids in this process.
- Breast milk forms softer curds in the infant's stomach than cow's milk (the basis for most formulas) and is more quickly assimilated into the body system.
- While it contains less protein than does cow's milk, virtually all the protein in breast milk is available to the baby. By contrast, about half the protein in cow's milk passes through the baby's body as a waste product.
- Similarly, iron and zinc are absorbed better by breastfed babies.
2. “Breastmilk doesn’t lose it’s nutritional value. Can you say that about the food YOU eat?”
- Even at a year, breastmilk continues to pack a powerful punch for nutritional value.
- In the second year (12-23 months), 448 mL of breastmilk provides:29% of energy requirements
- 43% of protein requirements
- 36% of calcium requirements
- 75% of vitamin A requirements
- 76% of folate requirements
- 94% of vitamin B12 requirements
- 60% of vitamin C requirements
Dewey KG. Nutrition, Growth, and Complementary Feeding of the Breastfed Infant. Pediatric Clinics of North American. February 2001;48(1), from Kellymom.com Breastfeeding Past Infancy Fact Sheet
3. “Breastmilk protects against disease for my baby. Don’t you want my (our) baby to be healthy?”
- Because the mother makes antibodies only to pathogens in her environment, the baby receives the protection it most needs-against the infectious agents it is most likely to encounter in the first weeks of life.
- Here are a few ways that breastmilk helps make a healthy baby:
- Breastfed babies also have less diarrhea and fewer gastrointestinal infections than babies who are artificially fed.
- Six months or more of exclusive breastfeeding reduces risk of food allergies.
- Breastmilk decreases a child’s risk of Crohn's disease and ulcerative colitis in adulthood.
- Breastfed babies have lower risk for developing recurrent wheezing when they are older (age 6 or more) – asthma
- They have less reflux
- They have less eczema
- Breastfeeding protects baby against respiratory infections
- Women who were formula-fed as infants have higher rates of breast cancer as adults. For both premenopausal and postmenopausal breast cancer, women who were breastfed as children, even if only for a short time, had a 25% lower risk of developing breast cancer than women who were exclusively formula-fed as infants.
4. “There are incredible health benefits for my breastfed baby. Do you really think it’s wise to limit my baby’s intellectual and physical potential?”
- Breastfed children have higher IQ
- Breastfeeding reduces a baby’s risk of SIDS by 50%
- Breastfeeding protects baby against vision defects. Breast milk is generally the main, if not the only source, of vitamin A during a child's first 24 months of life (or for the duration of breastfeeding).
- Suckling at the breast is good for a baby's tooth and jaw development, as the constant pulling at the jaw muscles promotes a well-formed jaw and healthy teeth.
5. “Breastfeeding improves my overall health. Who’s going to cook all of the meals and take care of the home if I’m not healthy? (I know...super snarky!)”
- Breastfeeding decreases mom’s risk of postpartum hemorrhaging as it stimulates contractions to shrink he uterus back to pre-pregnancy size.
- Breastfeeding reduces mom’s risk of osteoporosis
- Breastfeeding reduces mom’s risk of anemia, as breastfeeding postpones the return of menstruation for many women.
- Breastfeeding reduces mom’s risk of breast cancer. Women who breastfeed reduce their risk of developing breast cancer by as much as 25 percent. The reduction in cancer risk comes in proportion to the cumulative lifetime duration of breastfeeding. That is, the more months or years a mother breastfeeds, the lower her risk of breast cancer.
- Breastfeeding reduces the risk of uterine and ovarian cancer.
6. “Breastfeeding promotes mother/infant bonding and emotional well-being.”
- Babies feed for about 45 minutes per time in the first few months. This is nature’s way of making moms sit down and relax and promote her postpartum healing.
- Breast milk actually contains chemicals that suppress pain (endorphins). This is the perfect remedy for a child who accidentally hurts himself and is in need of some pain relief and comfort. It's like having a boo-boo-healing superpower!
- Babies can also feel the warmth of mom's skin, take in her scent and hear her heart beating. This helps to neurologically center thebaby after birth and help him/her adjust to the outside world.
- Breastfeeding also decreases a mother’s risk for postpartum depression.
7. “Breastfeeding can promote a positive relationship between mom and a supportive partner.”
- Partner support is crucial during breastfeeding, especially when there are challenges along the way.
- In the beginning, when baby is pretty much just eating and sleeping, mom and her partner can spend this time together, hanging out while the baby is feeding, getting to know one another as parents, not just partners.
- This is a great time to reconnect with your partner as the both of you get to know your baby, as this is a new time for your family.
- You are also a team during this time. Partners can make sure that all visitors offer positive breastfeeding comments, especially when breastfeeding is a challenge. No sabotaging comments allowed!
8. “Breastfeeding is definitely more convenient and less expensive than formula. I thought we were on a tight budget!”
- Breast milk, in any supply, is free. Ready-made formulas can cost families $800 to $1800 per child, annually.
- Nipples, bottles, bottle brushes and bottle bag inserts are additional costs, as well.
- Breastfed babies are ill less often, meaning that their parents miss fewer days at work and spend less on prescriptions, doctor's visits, and hospital stays.
9. “Breastfeeding, just like parenting, has bumps along the road and I won’t quit on my worst day.”
- As all thing that have to do with parenting, what works some days, doesn’t work on others and most things don’t go smoothly as planned.
- Your baby is born with a personality and a style that requires becoming familiar with and understanding.
- What works for some babies and children may not work for yours, so seek support anywhere you can find it: friends, family, lactation consultants, websites, Facebook groups, physicians, etc.
- Don’t quit on your worst day. Let 24 hours pass to gain some perspective and reach out for help during that time.
- Have an IBCLC evaluate your situation and provide a plan for overcoming your challenge.
10. “I promise you that my child won’t breastfeed until his high school graduation, but if he did, he’d probably be the smartest, healthiest graduate there!”
- Ok, maybe that’s a little too sassy, but you get the point. It is your choice to breastfeed for as long as mutually beneficial for you and your child. Every drop of breastmilk your child gets is liquid gold and you are a superstar for producing that for him/her! So stay strong, mama, and know that your ‘breast friends’ have your back! Happy nursing!
Top 10 Ways to Stop Caregivers from Overfeeding Your Breastfed Baby
How can a lactating parent ensure that her baby’s caregiver isn’t overfeeding, or unnecessarily throwing away, that precious liquid gold she spent time to pump out?
I hear it all the time.
Mom and partner get home from a much-needed date night to find out that grandma gave their 4-month old two 6oz bottles in 4 hours.
Mom picks up her baby from daycare to find out that her 6-month old took three 5oz bottles, plus the backup 5oz bottle in the freezer, in 8 hours. She pumped 12oz at work and thought that would be plenty for the next day. (which it is!)
Mom comes home from getting a haircut to find that her partner gave their 3-month old a 5oz bottle. The baby only ate 3oz, so her partner threw the extra 2oz away.
Who ever said there’s no crying over spilled (or wasted) milk never pumped breastmilk for her baby!
It’s hard work to pump… who has extra time when taking care of a newborn to pop on some plastic milk-extracting contraption and just sit for 15 minutes? Um… no one! So when a caregiver over feeds a baby, or throws away breast milk that could have been used at another time, it can be very frustrating and defeating for a mom. And as that extra freezer stash starts to dwindle because of misuse and over feeding, moms might feel their stress levels spike to an uncomfortable high.
So how can a mom ensure that her baby’s caregiver isn’t overfeeding, or unnecessarily throwing away, that precious liquid gold she spent time to pump out?
Top 10 Ways to Stop Caregivers from Overfeeding Your Breastfed Baby
Keep bottles in small increments (2-4oz, depending on the weight and age of your baby) and tell the caregiver to wait in between bottles to assess the baby’s mood (to see if he/she is really hungry) – Haley
Use the slowest flow nipple you can find and use the 1oz per hour rule (offer 1oz per hour that you are away from your baby) – Miranda
Pre-make bottles in small increments. For example, leave two 3oz bottles so caregivers don’t have to divide a 6oz bag into two separate bottles. – Shelly
Go over Kellymom’s article with your baby’s caregiver, How to bottlefeeding the breastfed baby, which talks about paced bottlefeeding – Tova and Megan
After baby has taken the bottle, try other soothing techniques (i.e. rocking, singing, swaying, take on a walk) rather than offering more breastmilk in an extra bottle.
Keep a few extra 1oz bags of breastmilk in the freezer or fridge. That way, if your baby’s caregiver really needs to offer your baby a little bit more, it is a small amount and won’t go to waste.
Talk to your baby’s caregiver about reusing breastmilk. While there are no definitive studies that state the exact amount of time that breastmilk must be used within (once the bottle has been fed from), most lactation consultants believe that if a bottle of breastmilk isn’t completely finished, it is safe to place it back in the fridge and the remainder used within 4 hours. (Kellymom.com article - Reusing Expressed Breastmilk)
Use the milk calculator to figure out how much your baby will need per bottle. Keep in mind, this is only accurate until your baby weighs 14lbs. After that, your baby’s breastmilk need plateaus at about 28-35oz per day. It won’t go up beyond that, so those 6-8oz bottles are really unnecessary.
Have a heart to heart discussion with your baby’s caregiver. Let him/her know how important it is to you that your baby isn’t overfed while away from you. Show empathy and explain that you understand how challenging it is to read your baby’s cues and that things are easier for you because you can always soothe your baby with your breast, which is something the caregiver cannot do. Explain how much milk your baby truly needs in a bottle and during the time you are gone. Anything over that is too much for your baby and makes it difficult for you to keep up. Come up with unique ways for him/her to bond with and soothe your baby, rather than just relying on giving more breastmilk in a bottle.
This advice came from a nanny, which was written so well I didn’t want to paraphrase it. ‘I nannies a breastfed baby for about a year and communication with the mom was very important. I also stuck to a schedule. If it was getting close to time for another bottle and I expected her home soon, I would text or call her to see if she wanted me to wait if she was on her way. Also, we would talk in the morning and she would let me know if she planned on coming home for lunch so I knew not to make a bottle. When I noticed that her son’s appetite was increasing, I would let her know that he was acting more hungry increased his bottles 1oz at a time. We also worked on adjusting his schedule so instead of 4oz every 2 hours, we found that 5oz every 3 hours kept him happy. That way he only needed 2 bottles while she was gone (10oz) instead of 3-4 bottles (12-16oz). A big help was her freezer milk in a variety of ounces. I was able to defrost what I needed to give her son without wasting any. As a breastfeeding mom myself, I did my best to respect the hard work she put into building a stash of milk for her son. – Catie.
Help a Mama Out: Nurturing Your Breastfeeding Relationship when Back at Work
Help a Mama Out Topic of the Week: What are your favorite ways to nurture your breastfeeding relationship when you work outside the home?
Sarah – When I was working out of the home, I pumped at the times my daughter would take a bottle. Then, when I came home I would exclusively nurse her. She was fine with 2 or 3 small breastmilk bottles a day, then nursed the rest of the time. She always preferred the breast and when it came time to wean, I was nervous….but at 13 months she just did and that was that!
Alicia – Comfort nursing on the weekends and morning nursing cuddle time. I always nurse as soon as we get home from work/daycare.
Alyssa – My favorite part of my working day (as a teacher) was when I sat down in the glider at daycare and nursed my son before taking him home for the night. We were always so happy to see each other and it helped wipe away any headaches from the day. Plus, I developed a friendship with his teacher and got to hear all about what he did that day, which was way better than just reading a quick note on a daily info sheet!
Jeanne – Co-sleeping helped us and a feed before I leave and ASAP when I get home. I also pump 3-4 times at work and always demand feed when I’m home.
Katie – We nurse in the evenings, when she wakes up in the middle of the night, and at least once more before I leave for work. It’s funny, as soon as I pick her up after work, I think her mind lights up with ‘milk!’ because she immediately wants to nurse regardless of when her last feeding was. I can tell that she misses that when we’re a part, as do I.
Janell – As soon as I get home, he’s on the boob. The rest of the night, he is on the boob. We spend all weekend with him on and off the boob. Time consuming, but I love the connection time and it forces me to sit down and breathe with my son.
Rachel – I sit with my daughter every evening after work. Even if she goes to sleep, we spend the entire evening and night together because we co-sleep. I make a point to forget about all of the housework I have to do and just relax with her because I know that she won’t be little forever!
Rachelle – One of my favorite things is when I get home from work, I shower (I’m a paramedic). After I shower, I fill the bath and my husband brings me the baby and we usually relax and nurse for 20-30 minutes. It is my wind-down time and it is quiet with few distractions. I love it!
Sarah – If possible, try to arrange a mid-day nursing session. I used a local daycare that I was able to visit at lunch and nurse, rather than pump. It greatly helped my supply and we were able to EBF for 13 months without any supplementation.
Amanda – I asked out childcare provider not to feed our little one within 90 minutes of when I planned to pick up. That way I could nurse as soon as I got there.
Eating Dinner for Breakfast to Help with Postpartum Weight Loss
Postpartum weight loss can be a bit tricky, especially when you are breastfeeding. While breastfeeding burns about 300-500 calories a day, this is not a time to limit your calories, as dropping below 1,500 calories a day has the potential to decrease a mother's milk supply. What this means is that a breastfeeding mother needs to net at least 1,500 calories a day, therefore she should aim to eat about 2,000 calories per day to keep a robust milk supply. Now, when a mother eats these calories, as well as the type of food she eats can make a difference in how those calories are used and burned throughout the day. My dear friend, Keegan Sheridan, is a naturopathic doctor and author of a fantastic blog at KeeganSheridan.com. Here is her most recent article about weight loss and eating breakfast for dinner.
Postpartum weight loss can be a bit tricky, especially when you are breastfeeding. While breastfeeding burns about 300-500 calories a day, this is not a time to limit your calories, as dropping below 1,500 calories a day has the potential to decrease a mother's milk supply. What this means is that a breastfeeding mother needs to net at least 1,500 calories a day, therefore she should aim to eat about 2,000 calories per day to keep a robust milk supply. Now, when a mother eats these calories, as well as the type of food she eats can make a difference in how those calories are used and burned throughout the day. My dear friend, Keegan Sheridan, is a naturopathic doctor and author of a fantastic blog at KeeganSheridan.com. Here is her most recent article about weight loss and eating breakfast for dinner.
For more information about breastfeeding and weight loss, please visit additional articles listed below.
Weight Loss: As Simple as Eating Your Dinner for Breakfast
Written by Keegan Sheridan, ND
For many years, I operated a private practice as a naturopathic doctor in Southern California, specializing in the treatment of digestive diseases and side-effects of cancer treatment. Although weight loss support was never a service that I proactively marketed, it was an all too common issue that I found myself needing to address with my patient population. Really, this wasn’t a surprise to me, given that close to 70% of all adults in this country are overweight or obese. Every doctor, no matter their specialization, can likely relate to my experience – given the epidemic of overweight and obesity in our country, the need to treat these diseases is fundamental to successfully addressing the vast majority of other symptoms and illnesses plaguing our society today.
Nourishing Meals Chicken Soup
The weight loss protocol that I created was conceptually quite simple and consisted of two basic recommendations:
- Decrease reliance on packaged and fast foods and increase consumption of whole foods
- Make breakfast the biggest meal of the day, lunch the next largest and dinner the smallest
I consciously avoided complicated rules and trends such as those found in diets like “The Zone” or “Atkins”. My goal was to create a mental shift in my patients from seeing a diet as a temporary thing to do to lose weight to a life-long way of approaching food in a healthy manner. Personally, I don’t have the time or interest to count calories, weigh my meals or eat the same frozen dinners over and over. Perhaps it was my own irritation with these trendy plans that played the biggest role in the advice I ultimately shared with patients.
To get started, I would often suggest a patient make one simple change: eat their dinner for breakfast and their breakfast for dinner. So, if they typically ate a chicken breast, green salad and slice of bread with butter for dinner and a bowl of cereal for breakfast, they’d just switch them up, simple as that. Although the idea of eating chicken breast and salad for breakfast was often a bit of a mental struggle, it was about as easy a change as you could make…no modifications to your grocery shopping list, no new recipes, no calorie counting. More times than not, when I would see them at their next appointment, they had lost weight…amazing but true. With the idea planted (and some nice weight loss results as motivator), I would then work with them to find more suitable meal ideas grounded in whole food ingredients that followed the same approach of eating the largest meal at breakfast and the smallest meal at dinner.
Last week when I came across a ***study recently published in the journal, Obesity, that followed this same approach I was incredibly excited. I was even more excited when I read the results of the study that found significant weight loss as well as other improvements in fasting glucose, insulin and triglyceride levels in the treatment group. How wonderful it was to see this approach studied and to see it demonstrate such positive and measurable results.
I have often joked that I discovered the next diet fad and have even come up with a few potential names, “The Dinner-Fast Diet”, “Eat Steak but Only at Breakfast Diet” or maybe, “The Upside Down Diet”. Too bad I don’t have a publishing deal…it seems like I really may be on to something!
*** Please note that the subjects in the study mentioned above were not breastfeeding and, therefore, consumed less than the recommended calories for a breastfeeding mother.
This article was first published on www.KeeganSheridan.com
Dr. Keegan Sheridan is a natural food and health expert, naturopathic doctor, and evangelist for healthy people and a healthy planet. She speaks and writes about the science, politics and evolution of natural food, health and medicine. Follow her on Twitter.
Additional articles about breastfeeding and weight loss found on our blog:
How to Lose Weight While Breastfeeding without Losing Your Milk Supply
Help A Mama Out: Ways Partners Can Bond with Baby Besides the Bottle
Help a Mama Out Topic of the Week: How does your partner bond with your baby besides giving a bottle?
So many partners who take my prenatal breastfeeding class want to know how they can start bonding with their babies besides giving bottles. Here are a few articles about partner support, as well as YOUR fantastic tips about how your partner and baby bond together.
Help a Mama Out Topic of the Week: How does your partner bond with your baby besides giving a bottle?
So many partners who take my prenatal breastfeeding class want to know how they can start bonding with their babies besides giving bottles. Here are a few articles about partner support, as well as YOUR fantastic tips about how your partner and baby bond together.
Lactation Matters: Fathers, Breastfeeding, and Bonding
Nancy Mohrbacher: The Mother’s Partner and the Breastfed Baby
Best for Babes: 14 Ways for Dads (and Partners) to be Engaged with their Breastfed Babes
Chelsea – He wears him in the baby carrier a lot and they like to read books together.
Shelly – When they were small, the only way we could get them to sleep was to put them in jammies on Daddy’s chest. It still works like a charm, almost at 13 months!
Erin – Babywearing and skin to skin! Too cute!
Cassandra – Every night he gives our son a coconut oil rub down…. It’s become such a bonding experience for them that when I even try to do this, my son whines and arches his back and crawls away.
Tiffany – He takes care of him in the morning while I sleep in. Change his diaper, play with him, and incorporate him into his ‘before-work’ exercise routine: calf raises with baby on shoulder, squats with baby in arms.
Ashley – Ours are bigger now, but when they were newbies and crying, he’d turn on Bunny Wailer and dance around the house with them. I still get teary when I hear Blackheart Man.
Lisa – Babywearing, bath time together, snuggles, walks, playing on the floor together.
Stephanie – Cuddles and babywearing. I heard a good quite recently about fathers. “It’s a father’s job to show his child that love doesn’t just come from food.”
Valerie – My wife spends lots of snuggle time with our daughter. Between babywearing, rocking, singing, and cuddling, she has quite the knack for soothing our baby.
Liz – My son hasn’t met daddy yet, as he is in Afghanistan, but when our daughter was a baby my husband would pretend fight with her. He would go all out…. Have her in the air, ‘slow mo’ kick her little baby feet into his face making some dramatic noises and rolling all over the bed with her. She wasn’t even a year old so it looked hilarious! Thank goodness I got a video of it! My hubby will also do diapers, carry, and co-sleep… the whole nine, but it’s his playtime bonding I love the most!
Mallory - My daughter has never had a bottle, so aside from helping with all of the other baby duties, he always reads her a bedtime story before I nurse her to sleep.
Tasha - Dad is a master burper and swaddler with our little one. He's also a pro at getting him to sleep because milk just doesn't do it some nights.
Jessica - By letting mommy sleep when he gets home in the mornings. My son love to fall asleep on his chest.
Thanks to everyone who responded to our questions on our San Diego Breastfeeding Center and The Boob Group Facebook pages. Check back every week for a new Help a Mama Out tip!
Here are a few more articles on our website, specifically dealing with partner support:
Advice for a Newly Breastfeeding Mama's Partner
Partner Support: Can it make or break your breastfeeding experience?
Breastfeeding Misconceptions: Does Baby Weight Loss Mean Mom Doesn’t Have Enough Milk?
How many times have you heard a so-called ‘fact’ from a family member, friend, healthcare professional, or online resource that has your ‘mama-radar’ going off at warp speed? Maybe something just doesn’t sound right. Maybe it goes against all of your mama-bear instincts. Maybe it is completely contradictory to what you heard the previous day. Well, it’s time to start busting those myths and misconceptions!
Today, we start our new series called Breastfeeding Misconceptions.
Every month we will be BUSTING common breastfeeding myths and misconceptions, hopefully making your breastfeeding experience that much easier!
How many times have you heard a so-called ‘fact’ from a family member, friend, healthcare professional, or online resource that has your ‘mama-radar’ going off at warp speed? Maybe something just doesn’t sound right. Maybe it goes against all of your mama-bear instincts. Maybe it is completely contradictory to what you heard the previous day. Well, it’s time to start busting those myths and misconceptions!
Today, we start our new series called Breastfeeding Misconceptions.
Every month we will be BUSTING common breastfeeding myths and misconceptions, hopefully making your breastfeeding experience that much easier!
Myth #1: If your baby loses weight in the first week, it means your milk supply is low.
Not true!
All babies lose weight after birth:
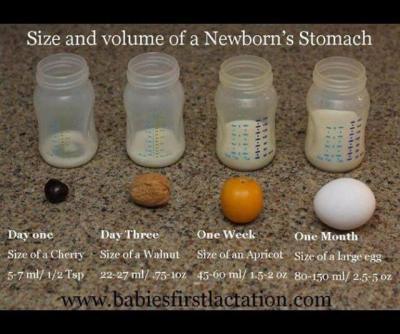
A newborn baby takes in approximately 5-7ml of colostrum per feeding in the first 24 hours. Babies are burning more calories than that as they attempt to breastfeed and expel that sticky, gooey meconium. Nature has provided the perfect amount of colostrum in those first few days to nourish your baby and while the quantity is small, the quality is jam-packed with every calorie, immunological property, protein, vitamin, and laxative that your newborn needs to poop and pee. Babies are expected to lose weight in those first few days. That doesn’t mean that mom’s supply is low.
Babies typically lose weight until mom’s ‘fuller milk’ comes in:
The amount of colostrum continues to grow as your milk transitions to ‘fuller milk’, which comes in around 2-5 days (depending on baby’s access to breast, effective sucking, birth interventions, etc.) Typical colostrum amounts are about 5-7 ml per feeding in first 24 hours, 7-15ml per feeding from 24-48 hours, and 22-27ml per feeding from 48-72 hours. Your baby will most likely lose weight until your ‘fuller milk’ comes in, but that doesn’t necessarily mean that you don’t have enough milk. What parents want to look for is that their baby is peeing and pooping (at least 1 of each per day of life) and baby’s weight loss plateaus once mom’s fuller milk has come in.
Here’s a great graphic of a baby’s stomach from Babies First Lactation and Education
Delayed milk supply doesn’t equal low milk supply:
There are several situations where a mother is at a higher risk for a delayed milk supply. As mentioned in this Best for Babes article, there are a number of factors that increase a mother’s risk for delayed milk supply. Some are beyond our control (or difficult to control): diabetes, obesity, thyroid problems, hypertension, PCOS, preterm birth, and anemia. There are also factors related to birth that can influence when a mother’s fuller supply comes in: cesarean birth, receiving lots of IV fluids, prolonged pushing stage, stress, cascade of interventions, hemorrhaging, mother-baby separation, just to name a few. If you are at a higher risk for having a delayed milk supply, it can be very helpful to speak with a lactation consultant within the first 24 hours after your baby is born. She can teach you ways to hand express and pump to help speed up the process of your fuller milk coming in, thereby DECREASING your risk for a low milk supply.
Lots of fluid during labor can cause greater weight loss in babies:
Studies have shown that mothers who have long periods of birth interventions (epidural, Pitocin, eventual emergency cesarean, etc.), tend to have more fluids during labor, thereby inflating baby’s birth weight and causing a large drop in baby’s weight in the first 24 hours. In those first 24 hours, we are looking for 1 pee and 1 stool (as a minimum.) For those babies that pee and stool multiple times in the first 24 hours, their weight loss is going to be greater, but that is not an indicator that mom’s supply is low. It just means they had a lot of fluids to expel after birth. Here are a few articles that explain this phenomenon. Dr. Jen: Newborn Weight and The Boob Group: Birth Interventions and Their Impact on Breastfeeding.
Baby may lose weight (or gain weight really slowly) because they are having a difficult time transferring mom’s milk:
There are many reasons why a baby might lose weight, sometimes continuing past the first week of life, even when mom has a full supply. Some of these include: engorgement (causing baby to have difficulties latching on), tongue-tie or lip tie, baby is recuperating after a difficult labor, baby is jaundiced, premature baby, etc. Again, when baby is losing weight due to these situations, it doesn’t always mean that mom’s supply is low. If her baby is having a difficult time transferring milk, then she should definitely meet with a lactation consultant to make sure she is doing everything she can to protect her milk supply until her baby can start to efficiently transfer milk from her breast.
Supplementation doesn’t equal formula:
If your milk supply is delayed, if your baby has elevated bilirubin, if your baby has lost more than 10% of his/her birth weight, that doesn’t automatically equal FORMULA supplementation. Mom may actually have enough of her own milk to supplement her baby with until baby’s weight is back on track. All she has to do is hand express or pump and see what extra she has. If mom doesn’t have enough of her own milk to supplement, then the hand expression or pumping (in addition to breastfeeding) will help to bring in her milk supply more fully. In the meantime, moms have other options. A mom can use milk bank breast milk or donor milk, if she prefers. For terrific information about milk banks, check out Human Milk Banking Association of North America and for milk sharing, check out Eats on Feets. The most important take away of this all…. When supplementation is necessary, it is imperative for a mom to increase her breast stimulation to help bring in her supply more fully. When her baby is getting a supplementation from another source, it is saying to mom’s body that she doesn’t have to make that amount of milk, which is totally not the case. The sooner mom’s fuller milk comes in, the sooner supplementation can decrease, so spend the extra time and effort… it will be worth it in the end.
Important note: When you might become concerned about your milk supply
While all of the above statements should illustrate why a mother should not be told that she has a low milk supply early on, there are some situations that might indicate that mom has a low milk supply (either temporarily or more long term.) If you are experiencing any of these situations, please connect with an IBCLC as soon as possible, as sometimes this can be a very temporary situation, as long as measures are taken quickly to protect mom’s milk supply. Here are some indicators that mom’s supply might be low:
Breasts did not grow and/or areola didn’t get darker during pregnancy
Breasts don’t feel heavier or fuller by 5-7 days postpartum
Fuller milk hasn’t ‘come in’ by 5-7 days postpartum
Baby is continuing to need supplementation to gain weight and mom is not making enough to supplement with her own milk
Mom has insufficient glandular tissue
Gerber to the Rescue (Or So They Want You To Think)
We’ve all been there.
You’ve been home with your new baby for a few days/weeks. It’s 2am and you’re tired and overwhelmed. You’ve never felt such bone-aching exhaustion. All you want to do is crawl in bed and sleep uninterrupted. Just for a few hours…. even ONE hour. But your baby is crying and won’t stop. You’ve tried everything – a fresh diaper, breastfeeding, you’ve shushed, swaddled and swung to the point of fatigue. And the baby won’t stop crying. You’ve woken your partner, called your mom or sister and none of the advice is helping. You’re worried that you’re doing something wrong or that you’re doing nothing right, that something is wrong with your little one, that you’re not making enough milk. You’d try almost anything at this moment to soothe your baby’s distress.
It’s exactly this vulnerability that formula companies prey upon when they make commercials like the one below:
The commercial for Gerber claims that the specially-created formula is effective in calming ‘excessive crying and colic.’ Nothing is more upsetting to a mother than the sound of her baby crying – we are biologically designed to physiologically respond to our own children’s sounds of distress, to do whatever we can to stop the baby from crying. Gerber is just PRAYING that a frustrated and exhausted mother will see this commercial and think that this new formula the answer to her struggles. Some moms may decide to introduce the formula to an exclusively breastfed baby, initiating the slippery slope of decreased supply and increasing ‘need’ for supplementation - just what formula companies are hoping for.
What Gerber fails to mention in the commercial is that the probiotic they have included (L. reuteri) has been studied and shown to exist in breast milk. Or that breast milk also has all the calories, protein, fat, carbohydrates and vitamins that your baby needs – AS WELL as antibacterial, antiviral, and antimicrobial factors specifically formulated to protect your baby. That breast milk contains all the probiotics AND prebiotics your baby may need. Or that human milk changes in composition as the baby grows, continually providing a unique superfood specific to YOUR baby.
Gerber also doesn’t explain to the new mom why her baby may be crying. The first three months of a baby’s life is often called the “fourth trimester” and should be treated as such. Just days ago, your baby was safely tucked in your womb, with constant warmth and soothing sounds and movements. Upon birth, the baby is thrust into his new environment, which is often cold and bright and always unfamiliar. Gerber doesn’t share the statistic that babies who are worn 3 or more hours a day cry 50% less than babies who aren’t. Gerber doesn’t remind the new mom that her 2-week old baby may be experiencing a growth spurtand the constant nursing and fussiness is a normal part of this, that the baby is doing all he needs to boost mom’s milk supply as he grows big and strong. Gerber doesn’t educate the mom on what she can add to or remove common allergenic or inflammatory foods (such as gluten, dairy, and soy) from her own diet to help soothe a colicky baby. (Check out our Boob Group podcast episode: GERD, Reflux and the Breastfed Baby for an explanation on symptoms, causes, and remedies for GERD, reflux, and colic.)
There are many reasons for a crying and colicky baby, and a number of solutions. One action that is never the answer is replacing any amount of breast milk with an artificial milk. Shame on Gerber for suggesting to an unsure and overwhelmed mother that her breast milk is lacking in something that could soothe her crying baby!